Hydrogen Peroxide as Liquid Disinfectant
Hydrogen peroxide
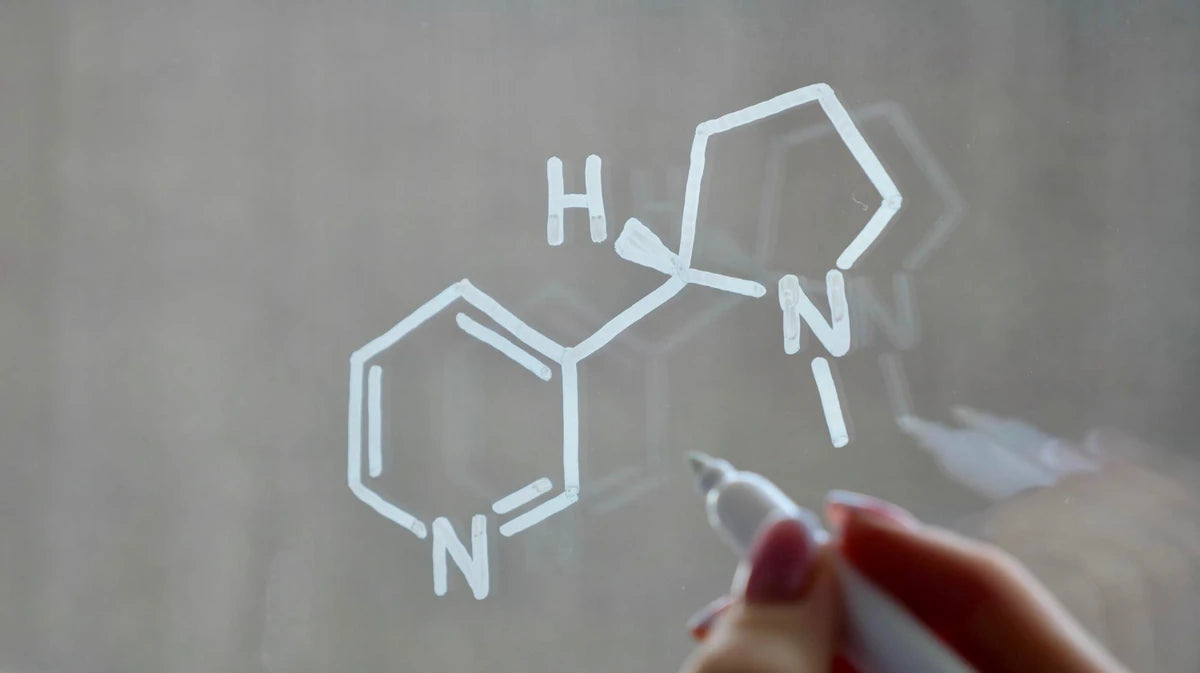
Hydrogen peroxide is used as a biocide in sterilization, disinfection and antisepsis. It is a colorless liquid. Commercial products of hydrogen peroxide are available in concentrations ranging from 3-90%. Hydrogen peroxide is environmentally friendly because it decomposes into water and oxygen. Although pure solutions are stable, stabilizing agents can be added to prevent deterioration. Hydrogen peroxide has a wide range of activity against viruses, bacteria, yeasts and bacterial spores. However, hydrogen peroxide's generally significant activity is against gram-positive rather than gram-negative bacteria. Although sporicidal activity increases significantly in the gas phase, higher concentrations of hydrogen peroxide (10-30%) and longer contact times are required. Hydrogen peroxide is a strong oxidizing agent because it produces free hydroxyl radicals. It is suggested that free hydroxyl radicals attack cell components such as DNA, lipids and proteins and particularly target sulfhydryl groups and double bonds.
Hydrogen peroxide is considered a high-level disinfectant for the disinfection of critical and semi-critical patient care units, and after cleaning the materials, 6% hydrogen peroxide concentrations are disinfected at room temperature for a minimum of 20 minutes of contact time. Mixtures of 7.5% hydrogen peroxide and 0.85% phosphoric acid concentrations can be used for high-level disinfection of endoscopes (compatible with hydrogen peroxide). The United States Food and Drug Administration (FDA) accepts 7.5% hydrogen peroxide for sterilization at 20°C and a contact time of 6 hours, and a contact time of 30 minutes for disinfection under the same conditions.
In recent years, the hydrogen peroxide gas plasma system has been developed for low-temperature sterilization. Gas plasmas are defined as the fourth state of matter and the process is carried out in a closed chamber under vacuum using microwave energy or radio waves to excite gas molecules (such as hydrogen peroxide) and produce charged particles. This method is effective against a wide range of microorganisms, including resistant bacterial spores. Like other sterilization processes, the effectiveness of this method can vary depending on lumen length, diameter, organic material, and inorganic salts. The hydrogen peroxide gas plasma system has been accepted by the FDA as a sterilization method. This system operates at temperatures lower than 140°F for heat-resistant materials. The sterilization time is 1 hour and, unlike ethylene oxide, it does not require an aeration step. The method is suitable for high-temperature-resistant materials and metals and can be used for a large number (>95%) of medical devices. However, it is not suitable for the sterilization of dialysis membranes used in microdialysis units that are not resistant to high temperatures, and endoscopes longer than 40 cm and smaller than 3 mm in diameter. It is also not recommended for the sterilization of paper, powder and liquids.
Formaldehyde fumigation is a traditional method used to control the decontamination of rooms and cabins. However, formaldehyde is a carcinogenic chemical substance for humans. In addition, it leaves aldehyde residues that need to be cleaned from equipment, walls and surfaces after the disinfection process. In recent years, one of the alternative “vapour-phase” decontamination methods within the scope of gas plasma techniques is hydrogen peroxide “vapour”. It is considered to be the most reliable of the existing decontamination methods. This method has been found to be effective against a large part of vegetative bacteria and fungi, Bacillus spp. and Clostridium botulinum spores.
In order to remove microorganisms from hemodialysis machines, a sufficient concentration of disinfectant and sufficient contact time are required. In determining the chemical disinfectant, the recommendations of the manufacturers should also be taken into consideration. Although chlorine-based disinfectants are suitable for the equipment, it is recommended to rinse them after 20-30 minutes following use because they have a corrosive effect. Disinfection with aldehyde derivatives (such as glutaraldehyde and formaldehyde) and peracetic acid does not have a corrosive effect on hemodialysis machines. Since formaldehyde, which is widely used, is a carcinogenic substance, the generally accepted disinfectants are glutaraldehyde and peracetic acid. Combinations of hydrogen peroxide and peracetic acid are used in hemodialysis disinfection. The use of disinfectants containing these compounds in the disinfection of dialyzers increased 10-fold between 1983 and 1997.
Dialyzers can be reused for the same patient in the next session after the washing and disinfection processes following the first use (reuse). It is effective and safe when the recommended rules for reuse are followed. Reuse process is applied especially to “hollow-fiber” dialyzers and although there are differences between units, a dialyzer is reused 10 times on average. Reuse process includes washing, cleaning, measurement of dialysis efficiency and disinfection steps. Sodium hypochlorite at a concentration of 1% or less, hydrogen peroxide at a concentration of 3% or less, peracetic acid at a concentration of 2% or less can be used in the cleaning process. Disinfection should be applied before the next use. Formaldehyde, renalin and glutaraldehyde are used for this purpose. If there is an abnormal color and appearance in the dialyzer after the process, it should not be reused. The disinfectant remains in the dialyzer until the next dialysis and the dialyzer must be completely cleaned of disinfectant before the next use. Rinsing protocols vary depending on the disinfectant used.
In contact lens disinfection systems, cleaning and disinfection of contact lenses are important in preventing eye infections. Hydrogen peroxide is effective against many microorganisms and especially resistant cysts of Acanthamoeba , which causes corneal infections . Multi-purpose solutions and hydrogen peroxide systems are applied for contact lens disinfection. In multi-purpose solutions, a single solution is used for storing, washing and disinfecting lenses. The hydrogen peroxide system is applied in two different ways. The reason for this is that hydrogen peroxide is toxic to the cornea and must be neutralized before the lens is inserted. There is no separate neutralization step in the single-step hydrogen peroxide solution. In this system, neutralization is performed during disinfection by using soluble catalase tablets or platinum-coated disks that catalyze the breakdown of hydrogen peroxide into water and oxygen. Two-step solutions include a separate neutralization step by adding sodium pyruvate or catalase after a certain disinfection period. In one-step systems, there is no burning that occurs when the lens is placed on the eye after being disinfected with the two-step system. However, one-step systems may provide less protection against Acanthamoeba keratitis because of the rapidity of the cyst-killing phase .
In recent years, povidone-iodine contact lens disinfection and cleaning systems have entered the market. The system includes the neutralization disinfectant and proteolytic enzyme stages of povidone-iodine with the addition of a separate agent. Although it has been found to be advantageous over the single-step hydrogen peroxide system, it does not provide continuous protection against pathogens because it has no residual antimicrobial activity after neutralization. Therefore, lenses must be re-disinfected after use of this system (if left for more than 24 hours).
Peracetic Acid
Peracetic acid (CH 3 COOH) is considered to be a more potent biocide than hydrogen peroxide because it is sporicidal, bactericidal, virucidal and fungicidal even at low concentrations (<0.3%). In addition to the safe degradation of peracetic acid or peroxyacetic acid into products such as acetic acid and oxygen, unlike hydrogen peroxide, they cannot be degraded by peroxidases and can remain active in the presence of organic molecules. It is suggested that peracetic acid denatures proteins and enzymes and increases cell wall permeability in a similar way to hydrogen peroxide.
Peracetic acid can inactivate gram-positive and gram-negative bacteria, yeasts and fungi at concentrations of less than 100 ppm and in about five minutes. In the presence of organic matter, 200-500 ppm peracetic acid is required to inactivate microorganisms. In viruses, the dosage increases to 12-2250 ppm. peracetic acid is a high-level disinfectant like hydrogen peroxide. Disinfection of critical and semi-critical hospital and patient care units is carried out at room temperature with a concentration of ≤ 1% peracetic acid and a contact time of 20 minutes. Since peracetic acid has a corrosive effect on metals such as copper, steel and iron, automation-based systems have been developed, especially for immersible endoscope disinfection, by diluting 35% peracetic acid to a concentration of 0.2% and adding a corrosive agent and buffer. The FDA has found 0.2% peracetic acid, 50-56°C and 12 minutes suitable for sterilization. However, peracetic acid can cause irreversible damage to the eyes, burn the skin and irritate the nose, throat and lungs when its vapors are inhaled.
An automatic device that uses peracetic acid to sterilize medical, surgical, and dental instruments became operational in 1988. The low-temperature sterilization method is widely used in the United States. Interchangeable parts help to sterilize rigid and flexible endoscopes. Connection systems that allow the endoscope channels to be flushed are suitable for many flexible endoscopes. Rigid endoscopes are placed in a lidded container. The chemical is filled with connection channels that flow directly into the cavity (lumen). As with other sterilization techniques, the system can only sterilize surfaces that come into contact with the chemical. For example, if the wrong connection system is used for bronchoscopes, bronchoscope-related infections can occur. The importance of channel connection systems for effective sterilization has also been demonstrated for rigid instruments.
The effect of peracetic acid on biofilms is controversial. Peracetic acid is responsible for the oxidation of chemicals in the biofilm. However, its killing function is not clear. Biofilms contain both strong and weak adherent compounds. Oxidation may be complicating the connection between adherent compounds via covalent bonds. Thin adherent biofilms are difficult to remove (as with water). In this case, peracetic acid may give a negative result together with water.
Although peracetic acid is considered an alternative to glutaraldehyde as a high-level disinfectant, it can sometimes bind biofilms on glassware. This activity is an undesirable result.
Medical textiles and clothing must be disinfected before use. Steam is generally used for this process. The disinfection effect is increased by adding peracetic acid to the steam. However, in some cases, it can shorten the life of textiles due to the damage it causes to the tissues in the material.
Peracetic Acid/Hydrogen Peroxide
The bactericidal properties of combinations of hydrogen peroxide and peracetic acid have been determined. These combinations can inactivate all microorganisms except bacterial spores within 20 minutes. A product containing a mixture of 1% hydrogen peroxide and 0.08% peracetic acid has been accepted by the FDA and is widely used in other countries for endoscope disinfection. This product is effective against Mycobacterium resistant to glutaraldehyde . Mixtures of 7.35% hydrogen peroxide and 0.23% peracetic acid have been accepted by the FDA for sterilization of endoscopes at 20°C and 180 minutes, and disinfection conditions of 15 minutes contact time at the same concentrations.
Baseline toxicological data may not be sufficient to determine the potential health effects of alternative chemicals to glutaraldehyde, such as peracetic acid, hydrogen peroxide, and ortho-phthalaldehyde (0.55%) (OPA). Hydrogen peroxide and peracetic acid have many advantages (Table 1). However, unknown problems may arise later. If a substance is not known to cause serious health problems, it is easy to assume that it is not harmful. Lack of information should be considered a warning rather than a safety concern.
High-level disinfection is a process that kills all microorganisms except bacterial spores. For the last 40 years, glutaraldehyde (2-4% in water) has been the primary chemical in high-level disinfection, but it has caused serious health problems such as dermatitis and asthma among workers.
OPA causes dermal and respiratory sensitization. The raw material used in the product is a dermal sensitizer. OPA has similar structural and reactive properties to glutaraldehyde. However, there is no published or unpublished information regarding peracetic acid and hydrogen peroxide indicating that these chemicals are sensitizers. Since these chemicals are not believed to cause allergic reactions or asthma, they can be considered a safe choice. However, this does not mean that alternative chemicals are not corrosive and toxic to the skin, eyes, mucosal membranes or respiratory tract.